Page |1 : Model of Health: Are Islamic Approaches to Healthcare Viable for the Developed World? Danika Tynes IDV 850 Dr. Pauly
A presentation at Dr. Danika Tynes, Ph.D. in August 2019 in Atlanta, GA, USA by Dr. Danika Tynes, Ph.D.
Page |1 : Model of Health: Are Islamic Approaches to Healthcare Viable for the Developed World? Danika Tynes IDV 850 Dr. Pauly
Page |2 Introduction In the West, perceptions of Islam are molded by popular discourse, media assumptions, and Western-oriented scholarly inquiry (Heyneman, 2004). Among those portrayals, discussion primarily revolves around “us vs. them,” “good Muslims vs. bad Muslims,” civilizational identities, geopolitics, and political Islam, with a close eye on current events in Egypt, Syria, Yemen, and other majority Muslim states (ibid; Huntington, 1999). Across the board, Islam is assumed to be characteristic of underdevelopment and almost synonymous with lack of modernity with little to no contribution to the modern world or how it is shaped (Esposito, 1999). However, just as modernity cannot be ignored by developing countries, the influence of the globalization of Islam cannot be shut out. In spite of these prevailing considerations of Muslim countries, this paper contends that the United States (i.e., a component and influencer of Western civilization) may be adopting several core Islamic principles in its healthcare reform and may do well to better understand the cultural characteristics that underlie the natural state of health that is a way of being in the Muslim communities that continue to grow. Herein, health policies of Muslim countries will be compared to those of the United States (U.S.). Nations are more similar in their focus on healthcare than any other function of government and the inclusion of morality in policy is more likely to appear in healthcare than any other realm (Carpenter, 2012). Islam purports that one’s health is a significant priority and it is one’s obligation to treat the body well, such as to eliminate parasites from pork in the diet, eschew liquor to maintain awareness of divine action at all times, or take proper medications when the need arises (Heyneman, 2004). Key messages delivered through Islam, such as the focus on preventive care over curative care, ambulatory care over hospitalization, and public
Page |3 care organizations over private ones are premises that are newly being adopted in major legislation in the United States (ibid). Islam’s attention to the connectedness between policy and religion as displayed in its guidance for healthcare, may provide some insights into the current transformations in global healthcare. This paper will review Islam’s religious references and guidance to achieving better health, document health policies enacted within Muslim countries, and compare such polices to those being implemented in the United States (U.S.). The research will seek to unfold whether commonalities exist and a framework can be started based on central tenets that could lend to a global healthcare structure that is not polarized by civilizational differences. Using case studies and longitudinal data on key healthcare indicators, this research will explore commonalities and divergences in health in the U.S. and in Arab nations. Literature Review Background on U.S.-Muslim Relations The Muslim world’s relationship with the West has been contentious for well over a thousand years owing to a natural struggle for territorial control and conquest (Esposito,1999). Those tensions that were political and ideological resulted in a back and forth over the millennia. It was in the 19th century, however, when the advantage fell squarely and definitively in the favor of the West owing to technological and military advances (Husain, 2003). It was then that imperialism and colonialism and all that was encompassed therein changed the relationship between the West and Muslim states forever. The demarcation can
Page |4 be firmly identified as before colonialism and after colonialism as the root of current day affairs. After WWII when de-colonization began, a shift was seen in the Muslim perception of ummah (“community” or “nation”) in favor of nation-states (ibid). But because these states were left off undeveloped and poor, the main survival tactic was to become dependent on foreign aid, which gave rise to further ideological conflicts (ibid). It appears that this rattling of identity launched the Muslim world into a search for a newly united one, where its proud history was restored, traditional society resumed, and it took the seat again as world power. Because the world is becoming smaller and there are more opportunities for the West to interact with Muslim countries through a variety of mediums (e.g., internet), identities continue to be challenged in an effort to not want anything to do with the colonizing West yet needing to be part of a increasingly globalized world (Huntington, 1993). Between colonization, de-colonization, and the ensuing identity crisis, the current day relationship between the West and Muslim countries, has declined significantly in the aggregation of several major events. In the 1970s, the Arab-Israeli War, the Arab oil embargo and the Iranian revolution invoked a new security and political concern for the West (Gerges, 1997). For example, the Western-oriented autocracy that was in place in Iran was rapidly and popularly overthrown and replaced by an Islamic theocracy, which represented a resurgence of Islam that served to take the West by surprise (Esposito, 1999). These events were followed by the hostage crisis in Iran during which time 52 Americans were held hostage for over one year having been overtaken, symbolically, at the United States (U.S.) embassy in Tehran (Gerges, 1997). These events amounted to Muslim countries being heightened on the U.S. security radar. What arguably sealed the current day relationship, however, was the 1993
Page |5 World Trade Center bombing (ibid; Husain, 2003). Bringing the war to U.S. soil and being politically strong armed to remove support for Israel and Egypt, was the catalyst for U.S. perceptions and approach to Muslim countries (with the U.S. being such a strong leader in the West, their partners followed). Of course, the events of 9/11 are infamous but the hostility between Muslim countries and the West had been reached and so attacks on the twin towers and the pentagon exacerbated and heightened the conflicts further. This back story serves to highlight that the influences Muslim states and the West have been cross-pollinating for centuries. It is not outside of reason to consider what influences have taken hold over time. Using Civilizations as the Level of Comparison Herein, healthcare in the U.S. and Islamic countries will be compared. This approach is predicated on existing theory of the appropriateness of civilizational comparisons. Samuel Huntington has argued that civilizations will be the central force behind shaping world politics and the source of conflict in the world will be cultural above other factors (Huntington, 1993; Husain, 2003). Post Cold-War, Huntington suggests that conflict and cohesion will best be understood through cultural identities. Huntington asserts that the West represents one civilization that has been particularly agitating to the others, especially Islamic, and suggests the West’s best course of action is to reaffirm their identity, return to it, and use that cohesion as strength to preserve it from outside challenges. Ultimately, Huntington suggests that the prevention of a global war or “clash” of civilizations relies upon the willingness of global leaders to maintain the “multicivilizational character” of global politics through acceptance and cooperation. Based upon Huntington’s identified civilizations, it is reasonable to assign civilization as the level of analysis.
Page |6 It has been argued that a weakness in Huntington’s thesis is the reductionism that is implicit in his civilization categorizations (Husain, 2003). For example, the coining of “the West and the rest” when referencing world politics, is an enormous over-simplification of the way the world works in practice. With globalization, teasing apart identity and culture is quite complex. However, using Islamic and Western civilizations as the level of analysis for comparison herein can provide at least some clues as to the intersection between them. Relevance of Institutions International institutions are defined as “relatively stable sets of related constitutive, regulative, and procedural norms and rules that pertain to the international system, the actors in the system (including states as well as nonstate entities), and their activities” (Duffield, 2007). Sandberg & Lindberg (2012) reinforce this broad definition and simplify it by putting forth a definition by North, wherein institutions are “rules of the game.” Institutions serve as a catalyst for much of the “mutual-aid society” structures (Ikenberry, 2011) and have provided a framework for collective action. Institutions are responsible to national governments being used as tools to coordinate interdependencies and reinforce norms of engagement. In the context of healthcare, there are many ways that institutions participate and drive health outcomes such as through formal institutions that enact policy or invest in healthcare infrastructure of a state. There are also social institutions such as religion and culture that determine, reinforce and drive norms and values. For example, a value held by a society could be that obesity reflects wealth, which would be reinforced by society in treating an obese woman more favorably and extending more options for marriage. That obesity value, however,
Page |7 might also associate to higher levels of diabetes or heart disease. Therefore, institutions, whether formal or informal, are key considerations in driving positive health outcomes. Background of Islam To best address the current health practices of Muslims, it is important to understand some fundamental tenets of the Islamic faith. Literally meaning “to surrender,” Islam is the world’s second largest religion next to Christianity (Husain, 2003). Islam enjoys well over one billion active Muslims (one who submits to the will of God or Allah) whose holy book, the Qur’an, was revealed to the prophet Muhammad who officially founded Islam in Madinah marking the beginning of the Islamic calendar in 622 C.E. (ibid; Esposito, 1999). Because Muhammad was the chosen messenger to reveal the word of God, he is held in the highest regard, not as a deity or one to be worshipped, but rather one to be emulated (Husain, 2003). Consequently, the Sunnah was documented to gather the ways of Muhammad, comprising of his sayings and deeds such that this collection stands second only to the Qur’an as the source of truth for Muslims (Esposito, 1999). Five articles of Islamic faith include: 1) Belief in Allah (God); 2) Belief in God’s angels (e.g., Archangel Gabriel); 3) Belief in God’s prophets (e.g., Adam, Muhammad); 4) Belief in God’s holy books; and 5) Belief in the day of judgment. The body of law that draws from Islamic articles is the “Shariah,” which is an immutable divine law that governs all aspects of being Muslim including economic, religious, and political life (Husain, 2003). At its core and intent, Islam is a very simple and straight-forward religion that is grounded in a commitment to peace for the community and within oneself. Islam became more complex as its timeline progressed and it became left to interpretation of man. Four legitimate successors of Muhammad, called “caliphs,” conquered
Page |8 many civilizations under their leadership lending to expansive territories exposed to Islam, such as Mesopotamia, Egypt, Syria, Palestine, Persia, North Africa and Iraq (Ibid; Esposito, 1999). By the 9th century, however, some Muslims believed in the Prophet Muhammad’s ways, the Sunnis, and others believed that the 4th caliph Ali ibn Abi Talib was the rightful religiopolitical leader, the Shi’ahs (or Shiites) (ibid). Over time, different degrees of adherence to Islam began to morph so that across the Islamic world, there are varying interpretations of Islam (Husain, 2003). Possibly the most important tenet of Islam, is that of “tawhid” or the unity and oneness of God and His complete sovereignty. This tenet has been a unifying force for Muslims as history has unfolded. Muslim Health Beliefs and Practices Religious beliefs generate normative values that translate to culture and ultimately impact behavior such as how one cares for their health (Yosef, 2008). Of paramount importance to Muslims is they “believe that God created human beings and gave them their bodies as gifts to be cared for” (ibid). Several core healthcare beliefs are fundamental to Islam to include hygiene, diet, and exercise. Key messages delivered through Islam include the focus on preventive care over curative care, ambulatory care over hospitalization, and public care organizations over private ones (Heyneman, 2004). Muslims believe in the purity of God and that purity can be achieved through cleanliness so the Qu’ran and Hadith both emphasize bodily hygiene (Yosef, 2008). Muslims, prior to their daily prayers are to wash their hands, face, head and feet and it is said to “cleanse your bodies, Allah will cleanse you” (Z. Ali et al., 1987). The Prophet Mohammad is said to have directed Muslims on proper teeth cleaning including brushing and flossing (Yosef, 2008)
Page |9 and that hair, fingernails, and cleaning after using the bathroom are all important (Z Ai et al., 1987). Diet is regarded as the key source of health for Muslims. The Qu’ran reads: “Eat of the good things which we have provided for your sustenance, but commit no excess therein” (ibid). Such a directive addresses moderation and eating for nourishment but not more. In addition, Muslims fast for one month for Ramadan during which time no food or drink is consumed before sundown each day (Yosef, 2008). Fasting is a way to purify the body and is one of the five pillars of Islam believed to promote the body and the spirit (Sherif & Lakhdar, 2010). Muslims reject drugs and alcohol because they stress the liver and fog the brain (ibid). The Qu’ran directs: “Forbidden to you are: dead animals - cattle-beast not slaughtered, blood, the flesh of swine, and the meat of that which has been slaughtered as a sacrifice for other than God…(Quran 5:3)…and intoxicants” (Quran 5:91-92). These expectations of Muslims are embedded in their religious thought and carry out in their daily activities reinforced by their culture. In addition to hygiene and diet, Islam places heavy emphasis on exercise. The five times daily prayers offers opportunities for movement with the standing and bowing (Yosef, 2008), which cannot be done readily or easily with and encumbered body. The Prophet Mohammed is said to have encouraged exercise, particularly outdoors as well as himself walking regularly and working outdoors (ibid). The Case of Iran in Health Policy Development Iran is an important example to review as a majority Muslim country that made sweeping healthcare changes. In 1979 a “Reconstruction Crusade” was launched under which religious
P a g e | 10 and state institutions were leveraged to provide better quality social and public welfare seeking to attain cleaner water and sanitation and establish over 2,000 new healthcare clinics (Heyneman, 2004). In 1982, sweeping organizational changes were implemented in the Ministry of Health in Iran and new policy placed priority on rural health, preventive care, ambulatory care and public hospitals (ibid). In 1984, the Iranian Primary Healthcare (PHC) network was established to focus on maternal/child health and prevention and control of disease. The PHC leveraged models of the World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) but only did so in alignment with Islamic doctrine. Institutions after the Iranian War were the mechanism by which the public health agenda was furthered. Mosques were the medium through which messages of the Iranian Health Minsistry were broadcast. These major shifts in approach to health in Iran were a naturally occurring evolution of leadership and institutional focus. The health outcomes achieved by 2000 were reduced child mortality, improved clean water and sanitation, increased immunizations, and more expansive family planning and preventive care (ibid). Iran’s policy interventions and innovations were keys in driving those positive healthcare outcomes demonstrating how existing institutions can be used to disseminate common messaging and reinforce existing doctrine. It is not surprising that Iran realized such successes in a short time because all of the policies that were implemented aligned with core Islamic principles so buy-in and mobilization was more accessible. This case of Iran points to the benefits of managing development through the use observation of social and indigenous values. Indeed, it is not that Iran merely adopted Western methods but that they modernized their approach to population health while observing their belief system ushered by embedded institutions.
P a g e | 11 United States Health Policy While Islamic culture provides a centralized and cohesive foundation to trace cultural healthcare emphases, the U.S. is much younger and far more heterogeneous, thus historical review is prohibitive for this discussion. U.S. health policy is broad and its evolution is complex, thus only current state will be reviewed here. On March 23, 2010, President Barrack Obama signed the Affordable Care Act (Health & Human Services, 2013). This recent law calls for sweeping healthcare reforms that seek to empower citizens to take greater stock in their own health by making access to quality healthcare a possibility for all. The timeline for implementation of the new law is particularly rapid but is not a ‘big bang’ approach and instead allows for phases to full enactment (ibid). In 2010, a Patient’s Bill of Rights went into effect and cost-free preventive services were made available to Americans who otherwise did not have access. In 2011, the Medicare program for older adults who opt into the government healthcare program was adjusted to also provide for free preventive services and expand access to brand-name medications. In 2012, Accountable Care Organizations (ACOs) were funded, which were provided government support for launching integrated, evidence-based, community-based care with a focus on improved population care outcomes. In 2013, a new Health Insurance Marketplace has been launched that allows all Americans to purchase a health plan despite pre-existing conditions, age, or other considerations that previously would have excluded the ability to have health insurance. The goal moving into 2014 and beyond is that all Americans will have affordable, quality healthcare (ibid). The key provision of the new law is to allow individuals in American society to participate in their own wellness.
P a g e | 12 The core features of the Affordable Care Act include more expansive coverage, reduced costs and more quality care. Coverage was expanded to end pre-existing condition exclusions, allow for young adults to remain on their parents’ insurance until the age of 26, end the ability for insurers to cancel insurance, and provide a mechanism to appeal any denials of payment by insurance companies. Cost structure was addressed to ban lifetime limits on benefits, make transparent any increases in healthcare rates so insurance companies cannot arbitrarily hike rates, and eliminate administrative costs from being folded into healthcare rates. Provisions for care made possible expanded preventive services, ability to choose one’s primary care provider, and the removal of barriers to emergency services (ibid). Since the signing of the Affordable Care Act, there has been tumultuous opposition to what seem to be positive aims. Political, economic and social arguments have been made in popular media consistently since March, 2010 often with polarizing outcomes for the U.S. population. Health policy in recent years in the U.S. has been a primary focus because of an aging population and foresight into rising costs that had the ability to spiral out of control and violating rights of equality of access to basic human needs that are a high value of American culture (Burchill et al., 2009). Comparisons of U.S. and Arab States Similarities and Differences in Health Policies The Islamic tenets of health are in direct alignment with the direction of U.S. health policy. Diet, hygiene, exercise and preventive care are high priorities for both and demand their resources and institutional focus. In addition, the direction of healthcare in the U.S. aligns with
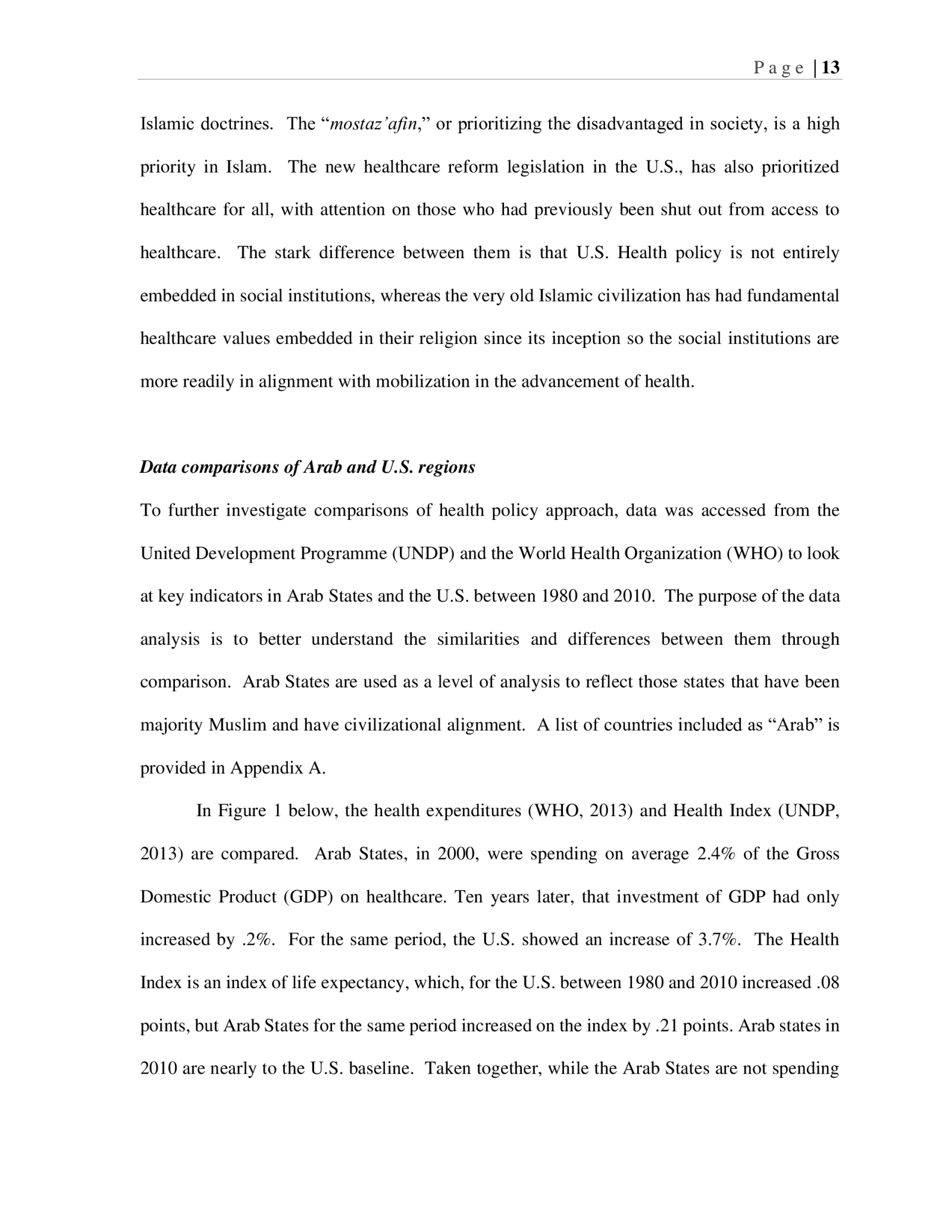
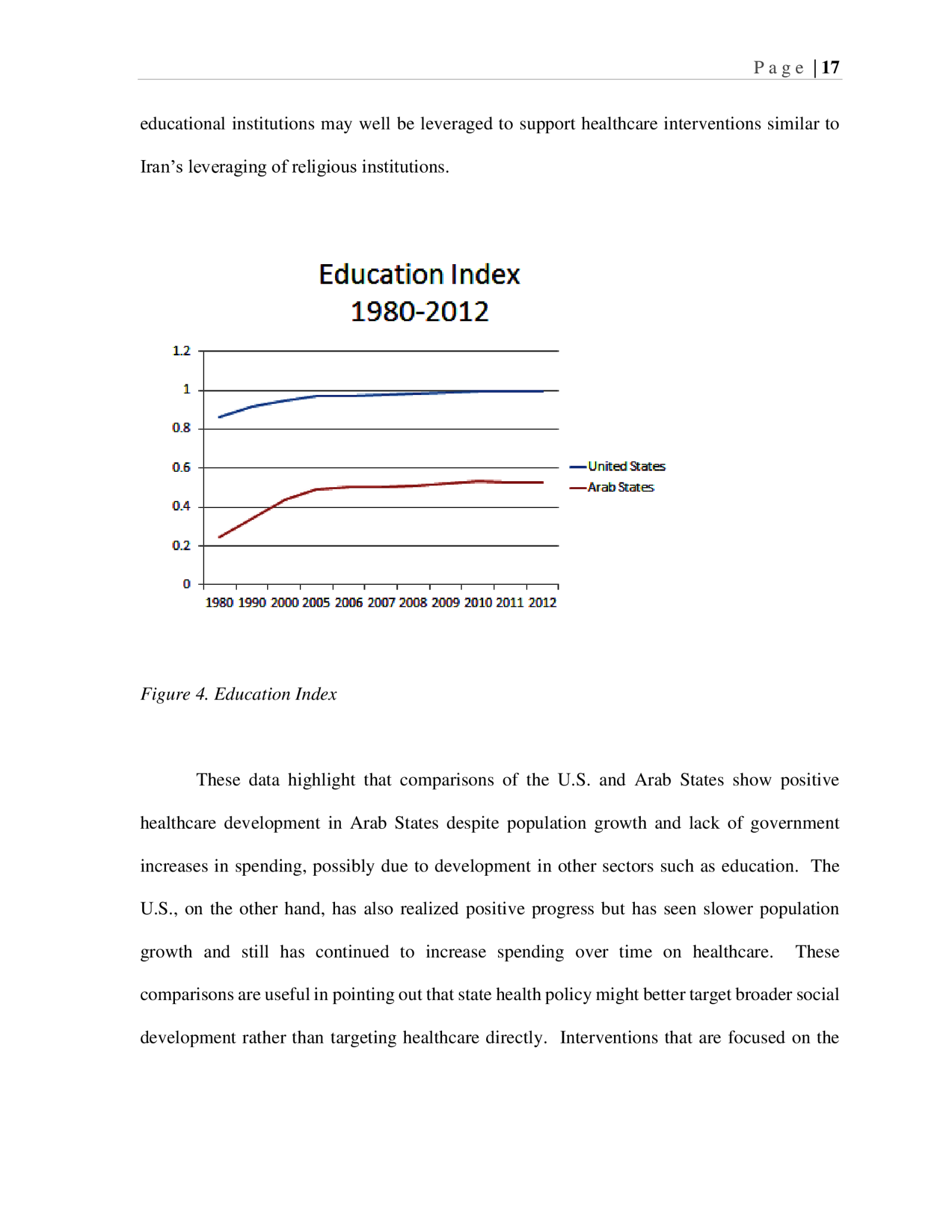
P a g e | 13 Islamic doctrines. The “mostaz’afin,” or prioritizing the disadvantaged in society, is a high priority in Islam. The new healthcare reform legislation in the U.S., has also prioritized healthcare for all, with attention on those who had previously been shut out from access to healthcare. The stark difference between them is that U.S. Health policy is not entirely embedded in social institutions, whereas the very old Islamic civilization has had fundamental healthcare values embedded in their religion since its inception so the social institutions are more readily in alignment with mobilization in the advancement of health. Data comparisons of Arab and U.S. regions To further investigate comparisons of health policy approach, data was accessed from the United Development Programme (UNDP) and the World Health Organization (WHO) to look at key indicators in Arab States and the U.S. between 1980 and 2010. The purpose of the data analysis is to better understand the similarities and differences between them through comparison. Arab States are used as a level of analysis to reflect those states that have been majority Muslim and have civilizational alignment. A list of countries included as “Arab” is provided in Appendix A. In Figure 1 below, the health expenditures (WHO, 2013) and Health Index (UNDP, 2013) are compared. Arab States, in 2000, were spending on average 2.4% of the Gross Domestic Product (GDP) on healthcare. Ten years later, that investment of GDP had only increased by .2%. For the same period, the U.S. showed an increase of 3.7%. The Health Index is an index of life expectancy, which, for the U.S. between 1980 and 2010 increased .08 points, but Arab States for the same period increased on the index by .21 points. Arab states in 2010 are nearly to the U.S. baseline. Taken together, while the Arab States are not spending
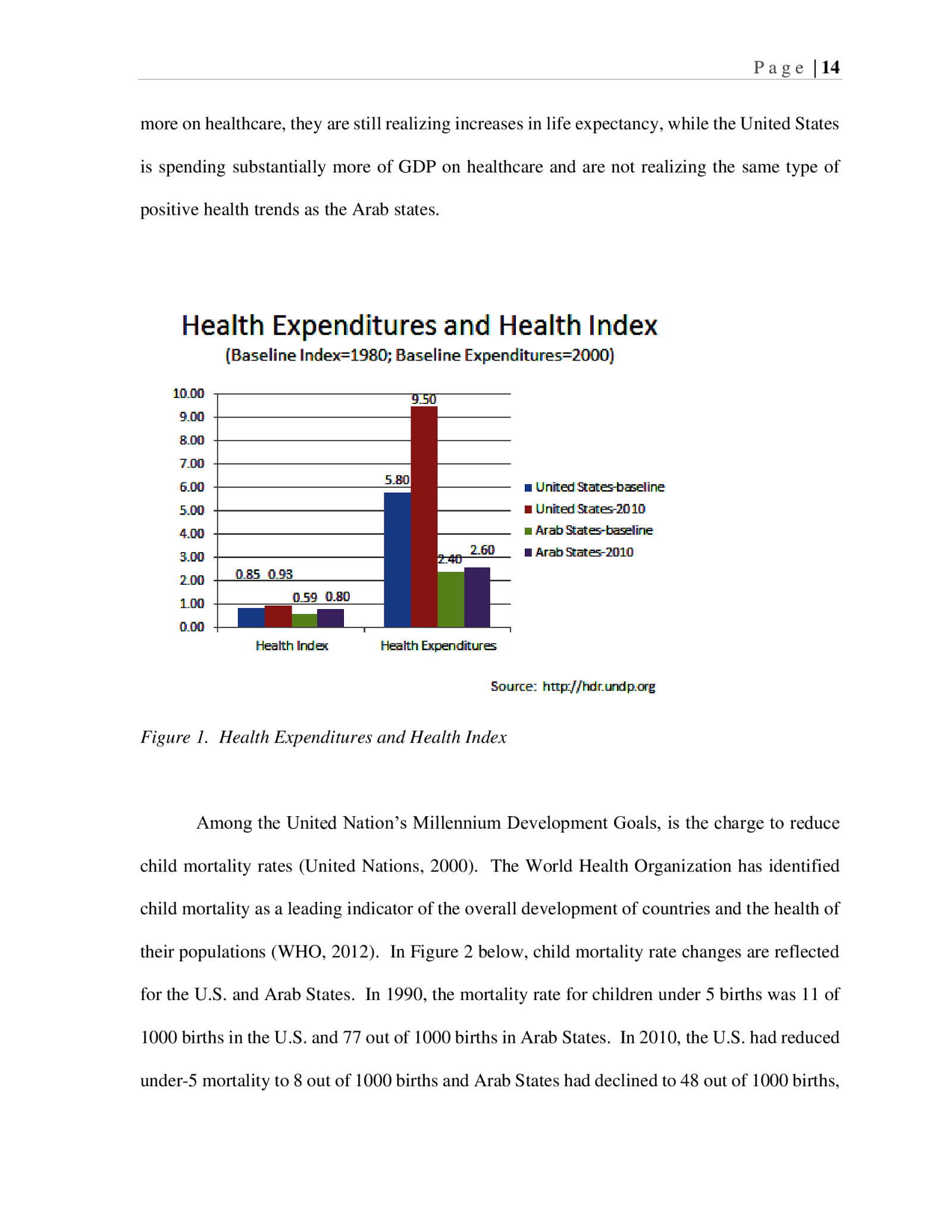
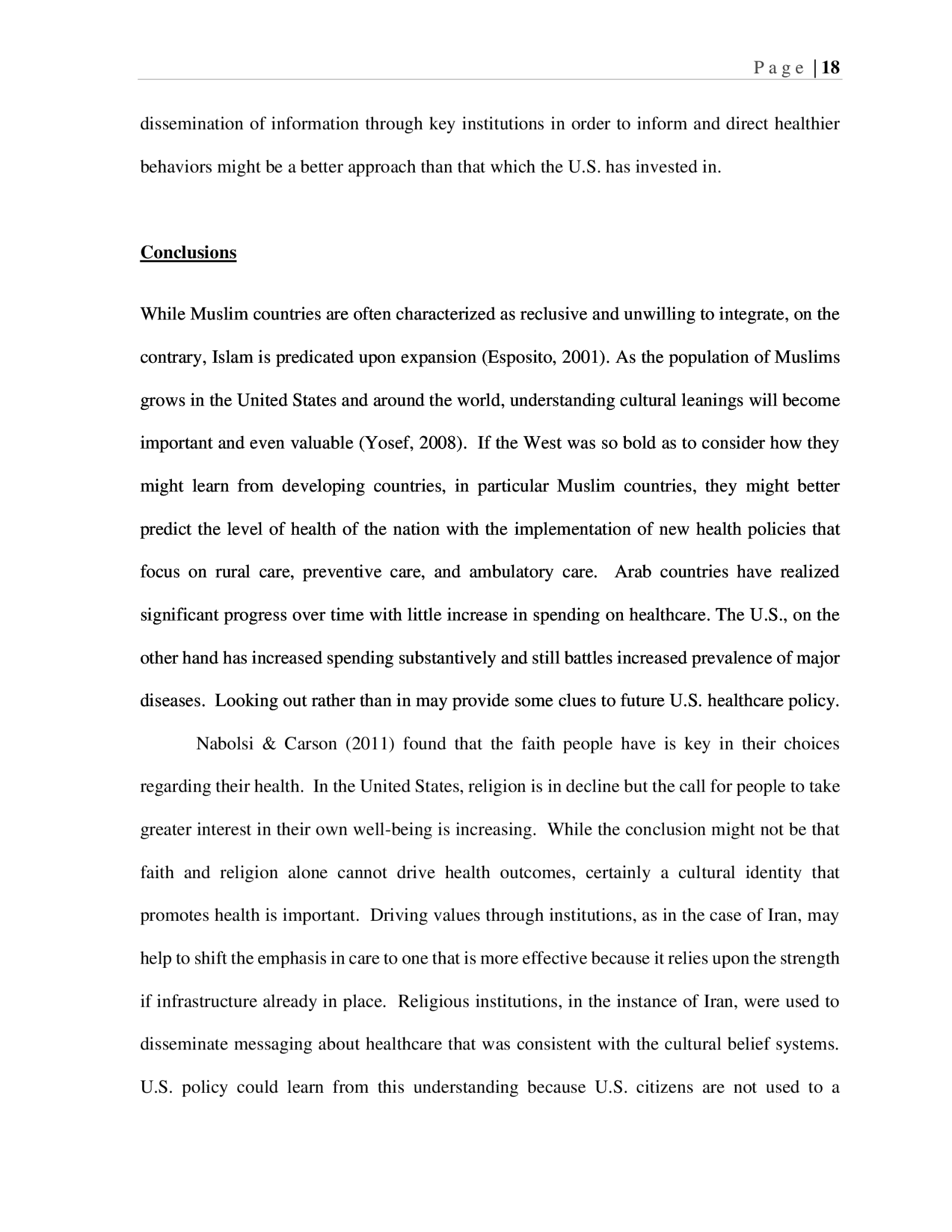
P a g e | 14 more on healthcare, they are still realizing increases in life expectancy, while the United States is spending substantially more of GDP on healthcare and are not realizing the same type of positive health trends as the Arab states. Figure 1. Health Expenditures and Health Index Among the United Nation’s Millennium Development Goals, is the charge to reduce child mortality rates (United Nations, 2000). The World Health Organization has identified child mortality as a leading indicator of the overall development of countries and the health of their populations (WHO, 2012). In Figure 2 below, child mortality rate changes are reflected for the U.S. and Arab States. In 1990, the mortality rate for children under 5 births was 11 of 1000 births in the U.S. and 77 out of 1000 births in Arab States. In 2010, the U.S. had reduced under-5 mortality to 8 out of 1000 births and Arab States had declined to 48 out of 1000 births,
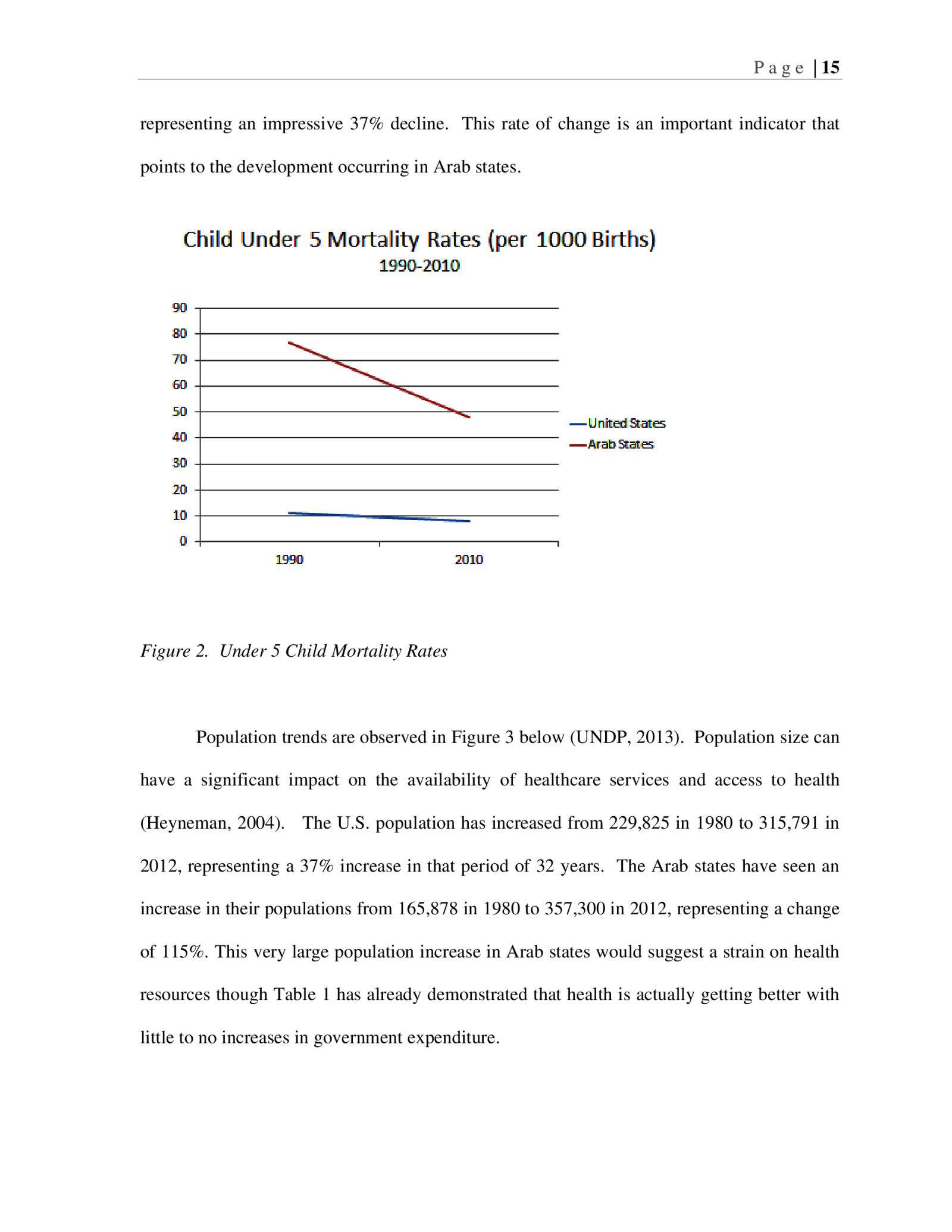
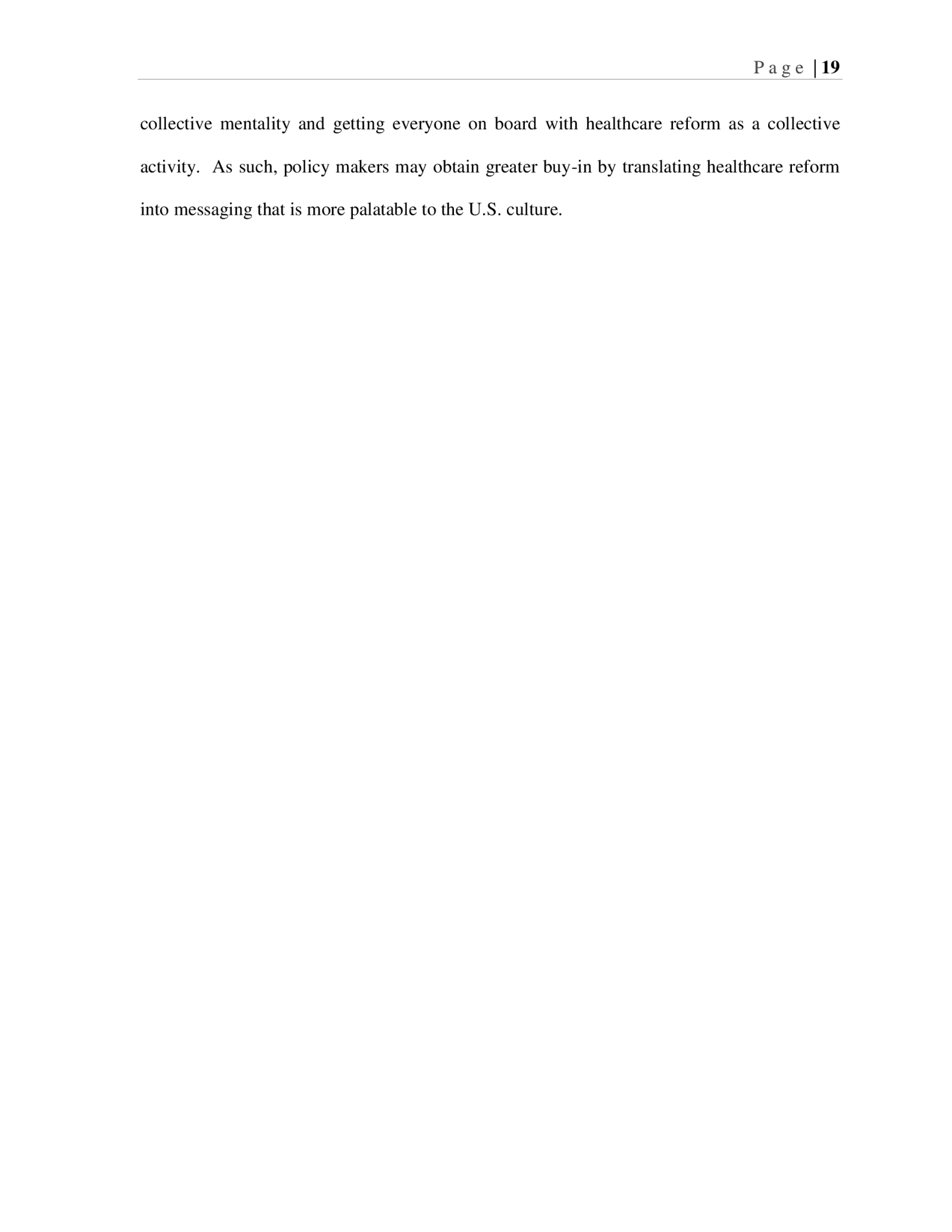
P a g e | 15 representing an impressive 37% decline. This rate of change is an important indicator that points to the development occurring in Arab states. Figure 2. Under 5 Child Mortality Rates Population trends are observed in Figure 3 below (UNDP, 2013). Population size can have a significant impact on the availability of healthcare services and access to health (Heyneman, 2004). The U.S. population has increased from 229,825 in 1980 to 315,791 in 2012, representing a 37% increase in that period of 32 years. The Arab states have seen an increase in their populations from 165,878 in 1980 to 357,300 in 2012, representing a change of 115%. This very large population increase in Arab states would suggest a strain on health resources though Table 1 has already demonstrated that health is actually getting better with little to no increases in government expenditure.
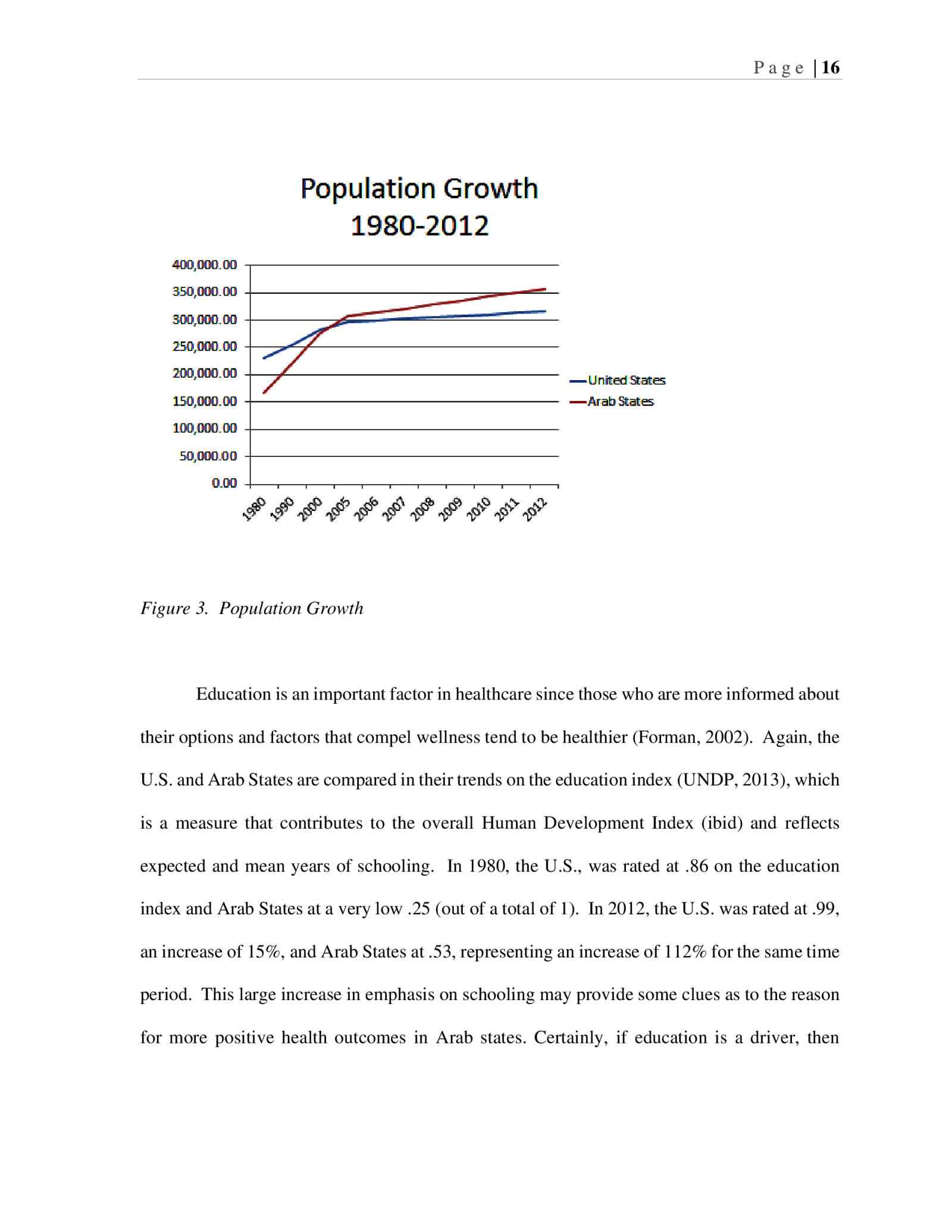
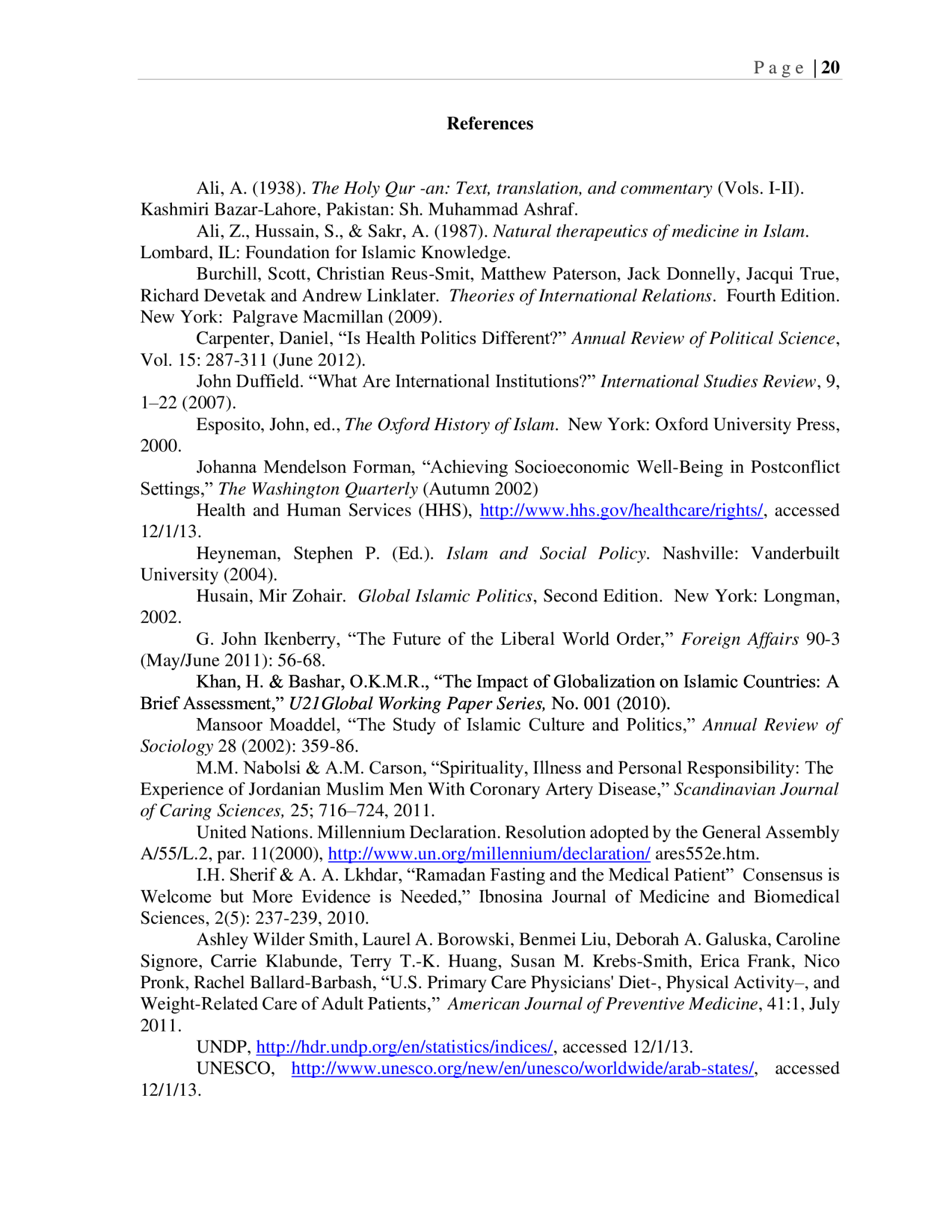
P a g e | 16 Figure 3. Population Growth Education is an important factor in healthcare since those who are more informed about their options and factors that compel wellness tend to be healthier (Forman, 2002). Again, the U.S. and Arab States are compared in their trends on the education index (UNDP, 2013), which is a measure that contributes to the overall Human Development Index (ibid) and reflects expected and mean years of schooling. In 1980, the U.S., was rated at .86 on the education index and Arab States at a very low .25 (out of a total of 1). In 2012, the U.S. was rated at .99, an increase of 15%, and Arab States at .53, representing an increase of 112% for the same time period. This large increase in emphasis on schooling may provide some clues as to the reason for more positive health outcomes in Arab states. Certainly, if education is a driver, then
P a g e | 17 educational institutions may well be leveraged to support healthcare interventions similar to Iran’s leveraging of religious institutions. Figure 4. Education Index These data highlight that comparisons of the U.S. and Arab States show positive healthcare development in Arab States despite population growth and lack of government increases in spending, possibly due to development in other sectors such as education. The U.S., on the other hand, has also realized positive progress but has seen slower population growth and still has continued to increase spending over time on healthcare. These comparisons are useful in pointing out that state health policy might better target broader social development rather than targeting healthcare directly. Interventions that are focused on the
P a g e | 18 dissemination of information through key institutions in order to inform and direct healthier behaviors might be a better approach than that which the U.S. has invested in. Conclusions While Muslim countries are often characterized as reclusive and unwilling to integrate, on the contrary, Islam is predicated upon expansion (Esposito, 2001). As the population of Muslims grows in the United States and around the world, understanding cultural leanings will become important and even valuable (Yosef, 2008). If the West was so bold as to consider how they might learn from developing countries, in particular Muslim countries, they might better predict the level of health of the nation with the implementation of new health policies that focus on rural care, preventive care, and ambulatory care. Arab countries have realized significant progress over time with little increase in spending on healthcare. The U.S., on the other hand has increased spending substantively and still battles increased prevalence of major diseases. Looking out rather than in may provide some clues to future U.S. healthcare policy. Nabolsi & Carson (2011) found that the faith people have is key in their choices regarding their health. In the United States, religion is in decline but the call for people to take greater interest in their own well-being is increasing. While the conclusion might not be that faith and religion alone cannot drive health outcomes, certainly a cultural identity that promotes health is important. Driving values through institutions, as in the case of Iran, may help to shift the emphasis in care to one that is more effective because it relies upon the strength if infrastructure already in place. Religious institutions, in the instance of Iran, were used to disseminate messaging about healthcare that was consistent with the cultural belief systems. U.S. policy could learn from this understanding because U.S. citizens are not used to a
P a g e | 19 collective mentality and getting everyone on board with healthcare reform as a collective activity. As such, policy makers may obtain greater buy-in by translating healthcare reform into messaging that is more palatable to the U.S. culture.
P a g e | 20 References Ali, A. (1938). The Holy Qur -an: Text, translation, and commentary (Vols. I-II). Kashmiri Bazar-Lahore, Pakistan: Sh. Muhammad Ashraf. Ali, Z., Hussain, S., & Sakr, A. (1987). Natural therapeutics of medicine in Islam. Lombard, IL: Foundation for Islamic Knowledge. Burchill, Scott, Christian Reus-Smit, Matthew Paterson, Jack Donnelly, Jacqui True, Richard Devetak and Andrew Linklater. Theories of International Relations. Fourth Edition. New York: Palgrave Macmillan (2009). Carpenter, Daniel, “Is Health Politics Different?” Annual Review of Political Science, Vol. 15: 287-311 (June 2012). John Duffield. “What Are International Institutions?” International Studies Review, 9, 1–22 (2007). Esposito, John, ed., The Oxford History of Islam. New York: Oxford University Press, 2000. Johanna Mendelson Forman, “Achieving Socioeconomic Well-Being in Postconflict Settings,” The Washington Quarterly (Autumn 2002) Health and Human Services (HHS), http://www.hhs.gov/healthcare/rights/, accessed 12/1/13. Heyneman, Stephen P. (Ed.). Islam and Social Policy. Nashville: Vanderbuilt University (2004). Husain, Mir Zohair. Global Islamic Politics, Second Edition. New York: Longman, 2002. G. John Ikenberry, “The Future of the Liberal World Order,” Foreign Affairs 90-3 (May/June 2011): 56-68. Khan, H. & Bashar, O.K.M.R., “The Impact of Globalization on Islamic Countries: A Brief Assessment,” U21Global Working Paper Series, No. 001 (2010). Mansoor Moaddel, “The Study of Islamic Culture and Politics,” Annual Review of Sociology 28 (2002): 359-86. M.M. Nabolsi & A.M. Carson, “Spirituality, Illness and Personal Responsibility: The Experience of Jordanian Muslim Men With Coronary Artery Disease,” Scandinavian Journal of Caring Sciences, 25; 716–724, 2011. United Nations. Millennium Declaration. Resolution adopted by the General Assembly A/55/L.2, par. 11(2000), http://www.un.org/millennium/declaration/ ares552e.htm. I.H. Sherif & A. A. Lkhdar, “Ramadan Fasting and the Medical Patient” Consensus is Welcome but More Evidence is Needed,” Ibnosina Journal of Medicine and Biomedical Sciences, 2(5): 237-239, 2010. Ashley Wilder Smith, Laurel A. Borowski, Benmei Liu, Deborah A. Galuska, Caroline Signore, Carrie Klabunde, Terry T.-K. Huang, Susan M. Krebs-Smith, Erica Frank, Nico Pronk, Rachel Ballard-Barbash, “U.S. Primary Care Physicians’ Diet-, Physical Activity–, and Weight-Related Care of Adult Patients,” American Journal of Preventive Medicine, 41:1, July 2011. UNDP, http://hdr.undp.org/en/statistics/indices/, accessed 12/1/13. UNESCO, http://www.unesco.org/new/en/unesco/worldwide/arab-states/, accessed 12/1/13.
P a g e | 21 WHO data: Government health expenditures: http://data.un.org/Explorer.aspx?d=15&f=docID:327, accessed 12/1/13. Yosef, Abdel Raheem Odeh, “Health Beliefs, Practice, and Priorities for Health Care of Arab Muslims in the United States, Journal of Transcultural Nursing,” Volume 19 Number 3, July 2008 284-291.
P a g e | 22 Appendix A. List of Arab States (UNESCO, 2013)